
Importance of early diagnosis
Leber’s hereditary optic neuropathy (LHON) is a rare, complex, and life-altering disease.Footnote1 The visual prognosis in LHON is generally poor.Footnote1 The majority of patients will end up legally blind with a visual acuity of 20/200 or worse, which results in a significant detrimental impact on their quality of life.Footnote1,Footnote2
Diagnosis is often delayed because of the lack of disease awareness and the inability to differentiate LHON from other conditions with similar characteristics, especially in the absence of family history.Footnote3
Diagnostic delays are common due to the relative rarity of LHON.3
Tests to confirm LHON
LHON is often mistaken for conditions such as brain tumour, multiple sclerosis, and optical neuropathies because of the nature of the LHON symptoms that develop in one eye.Footnote4–Footnote7
In addition to symptoms such as visual loss, a patient with LHON can often provide a history of visual loss in family members along the maternal line.Footnote8 Some of the tests that help confirm LHON are:
-
In LHON, there is an absence of dye leakage at the optic disc on fluorescein angiography. In the acute phase of the disease, an OCT reveals thickening of the retinal nerve fibre layer (RNFL) around the optic nerve and on subsequent examinations, in chronic phases (>12 months), it reveals thinning of the RNFL.
-
This is an emerging non-invasive technique for evaluating ocular microvasculature. With this method, the peripapillary retinal and vascular circulation can be evaluated three-dimensionally. Evaluation of vascular changes in LHON using OCTa may help us understand the pathophysiology of the disease, assess disease progression, and monitor the efficacy of treatment. OCTa is used to detect significant peripapillary microvascular changes over the disease course of LHON. In addition to the peripapillary region, OCTa studies have also provided evidence of pathology associated with the macular vasculature in different disease stages of LHON.
-
- An examination of the optic disc
- An electroretinogram (ERG) to measure the electrical responses in the retina
- A visual field test to characterise the area of vision loss (scotoma)
- An MRI or CT scan to rule out optic nerve inflammation or other causes of optic neuritis or CNS lesions
- A lumbar puncture may also be performed if a central nervous system infection is suspected
-
An mtDNA test traces a person’s mother-line using the DNA in their mitochondria.Footnote8,Footnote12 mtDNA is passed down by the mother unchanged, to all her children. Both men and women can therefore take an mtDNA test.Footnote8,Footnote12
LHON can usually be confirmed with an mtDNA blood test to reveal one of the three common mutations.Footnote8 Even if this test is negative, LHON may still be considered because approximately 10% of cases are not due to the three common LHON mutations.Footnote8,Footnote13 A complete mtDNA sequence analysis may be recommended if the clinical diagnosis of LHON remains a strong indication, or if there’s evidence of maternal transmission of blindness.Footnote8
DNA testing of primary LHON mutations is recommended in atypical presentations or in the absence of a clear family history of LHON.Footnote13
-
Recently, an autosomal recessive mode of inheritance for LHON was established when mutations in a nuclear encoded gene, DNAJC30, were identified.Footnote14 Given this, LHON can now be subdivided as mtLHON and arLHON, due to the important impact on genetic counselling.Footnote14 Clinical diagnosis for arLHON can be performed through patient-derived fibroblast cell lines obtained by skin biopsy.Footnote14
Molecular genetic testing
Molecular genetic testing approaches can include gene-targeted testing methods such as: targeted mtDNA analysis for pathogenic variants, multigene panel, and complete mtDNA sequencing.Footnote8
Please consult with your local genetics services to determine what testing options are available to you as this can differ depending on where you are in the UK. Steps 1 and 2 below can help detect the most common LHON mutations but may not be able to detect the rarer mutations. Please note that complete mtDNA and nuclear-mitochondrial screening require specialist referral.Footnote15
Requires referral to a specialist service15
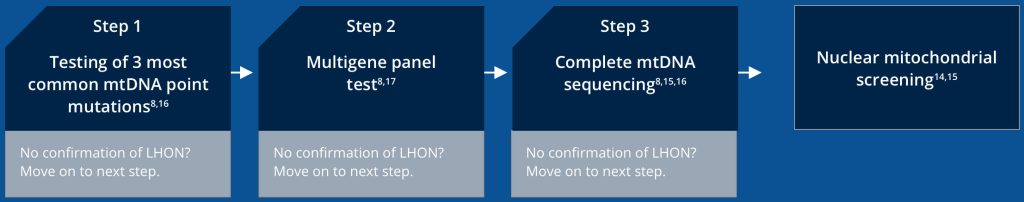
Step 1. Targeted mtDNA analysis8,16
The first step is to perform a targeted analysis for the three common mtDNA pathogenic variants observed in ~90% of individuals with LHON, all of which involve genes encoding complex I subunits of the mitochondrial respiratory chain.
These three variants are:
- m.3460G>A in MT-ND1
- m.11778G>A in MT-ND4
- m.11484T>C in MT-ND6
Step 2. Multigene* panel test8,17
If the targeted mtDNA test is inconclusive, a multigene panel would be the next step.
The panel used by the NHS Genomic Medicine Service (provided by Genomics England PanelApp) for diagnosis of LHON includes the MT-ND1, MT-ND4, and MT-ND6 genes (correct as of January 2023).
This test helps increase the chance of identifying disease-causing variants, at a reasonable cost, while limiting identification of variants of unknown significance.
Step 3. Complete mtDNA sequencing8,15,16
This is recommended if targeted testing and/or a multigene panel did not identify a pathogenic variant while clinical suspicion of LHON remains high.
Nuclear-mitochondrial gene screening14,15
Although rare, it is possible for LHON to be caused by recessive mutations in nuclear genes, therefore additional nuclear-mitochondrial gene screening should be considered before ruling out all possibility of diagnosis with LHON. For example, there is an autosomal recessive mode of inheritance for LHON caused by mutations in the nuclear encoded gene DNAJC30, which would not be detected through mtDNA screening alone. The distinction between mitochondrial and autosomal LHON has an additional impact on genetic counselling due to the variation in inheritance pattern.
Diagnostic pathway
Without a known family history of LHON, the diagnosis usually requires a neuro-ophthalmological evaluation and blood testing for mtDNA assessment.Footnote3,Footnote8 It is essential to exclude other possible causes of vision loss and other system abnormalities.Footnote3
Due to its rare nature, diagnosis of LHON is a long process. It often takes weeks or months from the onset of symptoms to receive a confirmed diagnosis.Footnote3
LHON patients are commonly misdiagnosed with optic neuritis and multiple sclerosis before they are properly diagnosedFootnote3

Adapted from Carelli V, et al. 2019.3
Referring your patient
Sudden sight loss demands urgent attention
Patients must get an LHON diagnosis sooner to get timely help and management of their condition.Footnote15
If you come across patients with sudden, unexplained and painless vision loss, refer them to any of the following without further delay.Footnote3,Footnote8
- An ophthalmologist who understands LHON
- A neuro-ophthalmologist
- A specialist LHON clinic
*Correct as per information on March 2023.
-
Theodorou-Kanakari A, et al. Adv Ther. 2018;35:1510–18.
Kirkman MA, et al. IOVS. 2009;50:3112–15.
Carelli V, et al. Eur Ophthalmic Rev. 2019;13 (Suppl 2).
Meyersen C, et al. Clin Ophthal. 2015;9:1165–76.
Yu-Wai-Man P, et al. Prog Retin Eye Res. 2011 81–114.
Fraser JA, et al. Surv Ophthalmol. 2010; 55:299–334.
Pfeffer G, et al. Neurology. 2013:81:2073–81.
Yu-Wai-Man P and Chinnery PF. Leber Hereditary Optic Neuropathy. GeneReviews® [Internet]. 2021. Available at: https:// www.ncbi.nlm.nih.gov/books/NBK1174/. Accessed: March 2023.
Sadun A, et al. Curr Treat Options Neurol. 2011:109–17.
Kızıltunç PB, et al. Turk J Ophthalmol. 2020;50:313–16.
Asanad S, et al. Ther Adv Ophthalmol. 2020, Vol. 12: 1–15.
International Society of Genetic Genealogy Wiki. Available at: https://isogg.org/wiki/Mitochondrial_DNA_tests. Accessed: March 2023
Yu-Wai-Man P, et al. J Med Genet. 2002;39:162–69.
Stenton SL, et al. J Clin Invest. 2021 Mar 15;131:e138267.
NHS Commissioning Board, 2013. Rare mitochondrial disorders service (all ages). Service specification 13/S(HSS)/h. Available at: https://www.england.nhs.uk/wp-content/uploads/2013/06/e13-rare-mitoch-dis.pdf. Accessed: March 2023.
NHS England. National Genomic Test Directory. Testing Criteria for Rare and Inherited Disease. June 2023. Available at: https://www.england.nhs.uk/wp-content/uploads/2018/08/Rare-and-inherited-disease-eligibility-criteria-version-5.2.pdf. Accessed: June 2023.
Genomics England PanelApp. Available at: https://panelapp.genomicsengland.co.uk/panels/530/. Accessed: March 2023.
Disclaimer: The information on this website is intended only to provide knowledge of Leber’s hereditary optic neuropathy (LHON). This website has been produced by Chiesi Pharmaceuticals. The website has been developed in accordance with industry and legal standards to provide information for healthcare professionals about LHON. Chiesi Pharmaceuticals makes every reasonable effort to include accurate and current information. However, the information provided in this website is not exhaustive.
 United Kingdom
United Kingdom  Global
Global  Sweden
Sweden  Greece
Greece  Norway
Norway